Pupillary light reflex
The pupillary light reflex is a reflex that controls the diameter of the pupil, in response to the intensity (luminance) of light that falls on the retina of the eye, thereby assisting in adaptation to various levels of darkness and light, in addition to retinal sensitivity. Greater intensity light causes the pupil to become smaller (allowing less light in), whereas lower intensity light causes the pupil to become larger (allowing more light in). Thus, the pupillary light reflex regulates the intensity of light entering the eye.[1]
Contents |
Mechanism
The optic nerve, or more precisely, the photosensitive ganglion cells through the retinohypothalamic tract, is responsible for the afferent limb of the pupillary reflex - it senses the incoming light. The oculomotor nerve is responsible for the efferent limb of the pupillary reflex - it drives the muscles that constrict the pupil.[1]
Neuron 1
The pupillary reflex pathway begins with the photosensitive retinal ganglion cells, which convey information to the optic nerve (via the optic disc). The optic nerve connects to the pretectal nucleus of the upper midbrain, bypassing the lateral geniculate nucleus and the primary visual cortex.
These "intrinsic photosensitive ganglion cells" are also referred to as "melanopsin-containing" cells, and they influence the circadian rhythms and the pupillary light reflex.
Neuron 2
From the pretectal nucleus, axons connect to neurons in the Edinger-Westphal nucleus, whose axons run along both the left and right oculomotor nerves.
Neuron 3
Oculomotor nerve axons synapse on ciliary ganglion neurons.
Neuron 4
Neuron #4 innervates the constrictor muscle of the iris.[1]
A Mathematical Description
Pupillary Light Reflex is modeled as a physiologically-based non-linear delay differential equation that describes the changes in the pupil diameter as a function of the environment lighting[2]:
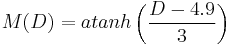
![\frac{dM}{dD}\frac{dD}{dt} %2B 2.3026 \; atanh \left( \frac{D-4.9}{3} \right) = 5.2 - 0.45 \; ln \left[\frac{ \Phi (t - \tau) }{4.8118~\times~10^{-10}} \right] \;\;](/2012-wikipedia_en_all_nopic_01_2012/I/187f9b9538bc3f50690e922774ef7345.png)
where  is the pupil diameter measured in millimeters and
is the pupil diameter measured in millimeters and  is the luminous intensity reaching the retina in a time
is the luminous intensity reaching the retina in a time  , which can be described as
, which can be described as  : luminance reaching the eye in lumens/mm2 times the pupil area in mm2.
: luminance reaching the eye in lumens/mm2 times the pupil area in mm2.  is the pupillary latency, a time delay between the instant in which the light pulse reaches the retina and the beginning of iridal reaction due nerve transmission, neuro-muscular excitation and activation delays.
is the pupillary latency, a time delay between the instant in which the light pulse reaches the retina and the beginning of iridal reaction due nerve transmission, neuro-muscular excitation and activation delays.  ,
,  and
and  are the derivatives for the
are the derivatives for the  function, pupil diameter
function, pupil diameter  and time
and time  .
.
Since the pupil constriction velocity is approximately 3 times faster than (re)dilation velocity,[3] different step sizes in the numerical solver simulation must be used:
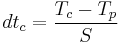
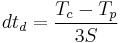
where  and
and  are respectively the
are respectively the  for constriction and dilation measured in milliseconds,
for constriction and dilation measured in milliseconds,  and
and  are respectively the current and previous simulation times (times since the simulation started) measured in milliseconds,
are respectively the current and previous simulation times (times since the simulation started) measured in milliseconds,  is a constant that affects the constriction/dilation velocity and varies among individuals. The higher the
is a constant that affects the constriction/dilation velocity and varies among individuals. The higher the  value, the smaller the time step used in the simulation and, consequently, the smaller the pupil constriction/dilation velocity.
value, the smaller the time step used in the simulation and, consequently, the smaller the pupil constriction/dilation velocity.
In order to improve the realism of the resulting simulations, the hippus effect can be approximated by adding small random variations to the environment light (in the range of 0.05 Hz to 0.3 Hz) as proposed by.[4]
Clinical significance
In addition to controlling the amount of light that enters the eye, the pupillary light reflex provides a useful diagnostic tool. It allows for testing the integrity of the sensory and motor functions of the eye.[1]
Under normal conditions, the pupils of both eyes respond identically to a light stimulus, regardless of which eye is being stimulated. Light entering one eye produces a constriction of the pupil of that eye, the direct response, as well as a constriction of the pupil of the unstimulated eye, the consensual response. Comparing these two responses in both eyes is helpful in locating a lesion.[1][5]
For example, a direct response in the right pupil without a consensual response in the left pupil suggests a problem with the motor connection to the left pupil (perhaps as a result of damage to the oculomotor nerve or Edinger-Westphal nucleus of the brainstem). Lack of response to light stimulation of the right eye if both eyes respond normally to stimulation of the left eye indicates damage to the sensory input from the right eye (perhaps to the right retina or optic nerve).[1]
Emergency room physicians routinely assess the pupillary reflex because it is useful for gauging brain stem function. Normally, pupils react (i.e. constrict) equally. Lack of the pupillary reflex or an abnormal pupillary reflex can be caused by optic nerve damage, oculomotor nerve damage, brain stem death and depressant drugs, such as barbiturates.
Normally, both pupils should constrict with light shone into either eye alone. On testing each reflex for each eye, several patterns are possible.[6]
- Optic nerve damage on one side: (Example in parens.: Left optic nerve lesion)
- The ipsilateral direct reflex is lost (Example: when the left eye is stimulated, neither pupil constricts, as no signals reach the brain from the left eye due to its damaged optic nerve)
- The ipsilateral consensual reflex is INTACT (because light shone into the right eye can signal to the brain, causing constriction of both pupils via the normal oculomotor nerves)
- The contralateral direct reflex is intact (because light shone into the right eye can signal to the brain, causing constriction of both pupils via the normal oculomotor nerves)
- The contralateral consensual reflex is lost (because light shone into the eye on the damaged side cannot signal to the brain; therefore, despite the right eye's motor pathway (oculomotor nerve) being intact, no signals from the left eye are able to stimulate it due to the damage to the sensory pathway (optic nerve) of the left eye)
- Oculomotor nerve damage on one side: (Example in parens: Left oculomotor lesion)
- The ipsilateral direct reflex is lost (Example: when the left eye is stimulated, only the right pupil constricts)
- The ipsilateral consensual reflex is lost (Example: when the right eye is stimulated, only the right pupil constricts)
- The contralateral direct reflex is intact (because light shone into both eyes can still signal to the brain, and the pupil on the undamaged side will still be able to constrict via its normal oculomotor nerve)
- The contralateral consensual reflex is intact (because light shone into the left eye can still signal to the brain via the normal optic nerve, causing attempted constriction of both pupils; the contralateral pupil constricts via its normal oculomotor nerve, but the ipsilateral pupil is unable to constrict due to its damaged oculomotor nerve)
See also
References
- ^ a b c d e f Purves, Dale, George J. Augustine, David Fitzpatrick, William C. Hall, Anthony-Samuel LaMantia, James O. McNamara, and Leonard E. White (2008). Neuroscience. 4th ed.. Sinauer Associates. pp. 290–1. ISBN 978-0-87893-697-7.
- ^ Pamplona, V. F., Oliveira, M. M., and Baranoski, G. V. G. (2009). Photorealistic models for pupil light reflex and iridal pattern deformation. ACM Trans. Graph. 28, 4 (Aug. 2009), 106:1-106:12. DOI= http://doi.acm.org/10.1145/1559755.1559763
- ^ Ellis, C. J. (1981). "The pupillary light reflex in normal subjects". British Journal of Ophthalmology 65 (11): 754–759. doi:10.1136/bjo.65.11.754. PMC 1039657. PMID 7326222. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1039657.
- ^ Stark, L. W. (1939). Stability, Oscillations, and Noise in the Human Pupil Servomechanism. Proc. of the IRE, [S.l.], v.47, n.11, p.1925–1939
- ^ "Cranial Nerve III—Oculomotor Nerve". yale.edu. http://www.med.yale.edu/caim/cnerves/cn3/cn3_12.html. Retrieved 2008-07-27.
- ^ Colman, Andrew M. (August 2001). A Dictionary of Psychology. Oxford University Press, USA. ISBN 0-1986-6211-4.
External links
- Animation of pupillary light reflex
- MeSH Reflex,+Pupillary
- A pupil examination simulator, demonstrating the changes in pupil reactions for various nerve lesions.
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||